Introduction
Alpha thalassemia major is generally fatal in utero or shortly after birth without aggressive red cell transfusion therapy both pre- and postnatally. The Society for Maternal-Fetal Medicine has released evidence-based practice guidelines for the diagnosis and management of fetal anemia, largely focused on red cell alloimmunization, with intrauterine transfusion typically starting at 18 weeks gestational age.((SMFM) et al., 2015) Early initiation of intrauterine transfusion allows quick correction of anemia and a prolonged reduction of hemoglobin Bart's concentration leading up to birth.(Chmait, Baskin, Carson, Randolph, & Hamilton, 2015) Long-term transfusion regimens postnatally invariably lead to iron overload, which can lead to organ dysfunction.(Taher & Saliba, 2017) Minimal data is currently available regarding the pattern of iron overload in young patients with alpha thalassemia major given the rarity of the disease itself and variations in iron overload monitoring.
Methods
We reviewed patients with alpha thalassemia major treated at our center who had iron overload evaluations prior to 10 years of age. Diagnoses were confirmed by genetic testing. Iron deposition measurements were collected using multiple gradient echo pulse sequences on 1.5 Tesla magnets.
Results
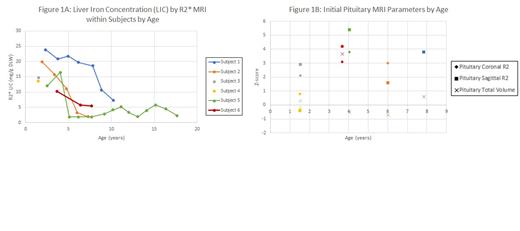
Six subjects were included in the study. All but one subject received several intrauterine transfusions and were delivered at term. The last subject did not receive any intrauterine transfusions and was born at 24 weeks gestational age. Subjects were routinely transfused postnatally to keep fast migrating hemoglobin below 10%. Initial MRI was done prior to 4 years of age and as early as 1.5 years. All subjects had moderate to severe iron overload based on liver iron concentration (LIC) by R2* MRI, which decreased significantly after starting chelation in the four subjects who had subsequent MRI assessments (Figure 1A). Pancreatic iron was also elevated in all subjects, and none had cardiac siderosis. All but one subject had pituitary R2 by Z-score for age and sex greater than 2 in the coronal and sagittal planes, indicating pituitary siderosis, but none had pituitary volume loss (Figure 2B).
Discussion
This study shows significant extrahepatic iron deposition (pancreas, pituitary) at a very young age indicating exposure to toxic reactive ferrous iron (Fe 2+). The pancreas is known to load temporally before the heart.(Noetzli, Papudesi, Coates, & Wood, 2009) None of the subjects in this study had cardiac iron by MRI, probably reflecting slower cardiac loading and lowering of Fe 2+ by chelation. It is very rare to have cardiac loading from transfusion in patients less than 2 years old.(Berdoukas et al., 2013) It is reassuring that none of the patients had pituitary volume loss, which has been associated with pituitary dysfunction,(Noetzli et al., 2012) although we know very little about pituitary function and iron in very young children. Our observation that some subjects had loading at 1.5 years old suggests there is significant circulating Fe 2+ in this population and the pituitary may be at risk.
Chelation is rarely started prior to 2 years of age due to concerns about theoretical effects of chelation on neurodevelopment.(Coates, 2019) Despite significant levels of iron overload seen in initial assessments, hepatic iron rapidly improved with chelation despite aggressive red cell transfusion in this cohort. There are many unknowns here, including effects of prenatal iron exposure from transfusion, the extent to which iron seen by MRI signifies organ damage, and response of extrahepatic iron to chelation. However, the effects of iron deficiency on brain development are well documented(Idjradinata & Pollitt, 1993; Lozoff et al., 2013) and the possible effects of chelators on the newborn/infant brain could be serious. Long-term pituitary iron data are still needed to support earlier implementation of iron chelation in this population.
Disclosures
Carson:Chiesi: Speakers Bureau. Wood:Philips Medical Systems: Other: Support-In-Kind, Research Funding; Imago Biosciences: Consultancy; Hillhurst: Consultancy; Agios: Consultancy; Celgene: Consultancy; Pharmacosmos: Consultancy. Coates:Agios Pharmaceuticals: Consultancy; Chiesi: Consultancy; Bristol Myers Squibb: Consultancy.